Treatments for Dry AMD
Diet and Nutrition
Diet and nutrition treatments for dry macular degeneration focus on boosting retinal health through antioxidant-rich foods and targeted supplements.
Research—most notably from the AREDS and AREDS2 studies—shows that daily supplementation with vitamins C and E, zinc, and the carotenoids lutein and zeaxanthin can help slow progression in intermediate dry AMD.
A balanced diet rich in leafy greens, colorful fruits, fish, and nuts provides these essential nutrients naturally, while avoiding refined carbohydrates, saturated fats, and processed foods may help reduce oxidative stress and inflammation.
Although no dietary intervention reverses existing damage, these nutritional strategies form an important part of managing the condition and potentially preserving vision
Intravitreal injections (Dry AMD)
Current research on intravitreal injections for dry macular degeneration is evolving rapidly. Unlike wet AMD—where anti‑VEGF treatments are well established—injections for dry AMD primarily target the complement cascade, a key pathway in the slow degeneration seen in geographic atrophy. Notably, intravitreal complement inhibitors such as pegcetacoplan and avacincaptad pegol have attracted considerable attention.
Clinical trials (including the Phase II FILLY study and subsequent Phase III trials) have shown that these agents can reduce the progression of atrophic lesions by slowing the enlargement of geographic atrophy, although the benefit comes with potential risks such as a modest increase in conversion to neovascular (wet) AMD.
While these treatments do not restore lost vision, they represent a significant step toward modifying the course of dry AMD. Overall, the evidence is promising but mixed, and further long-term studies are necessary to refine dosing strategies, fully assess safety profiles, and determine which patients are most likely to benefit from this therapeutic approach.
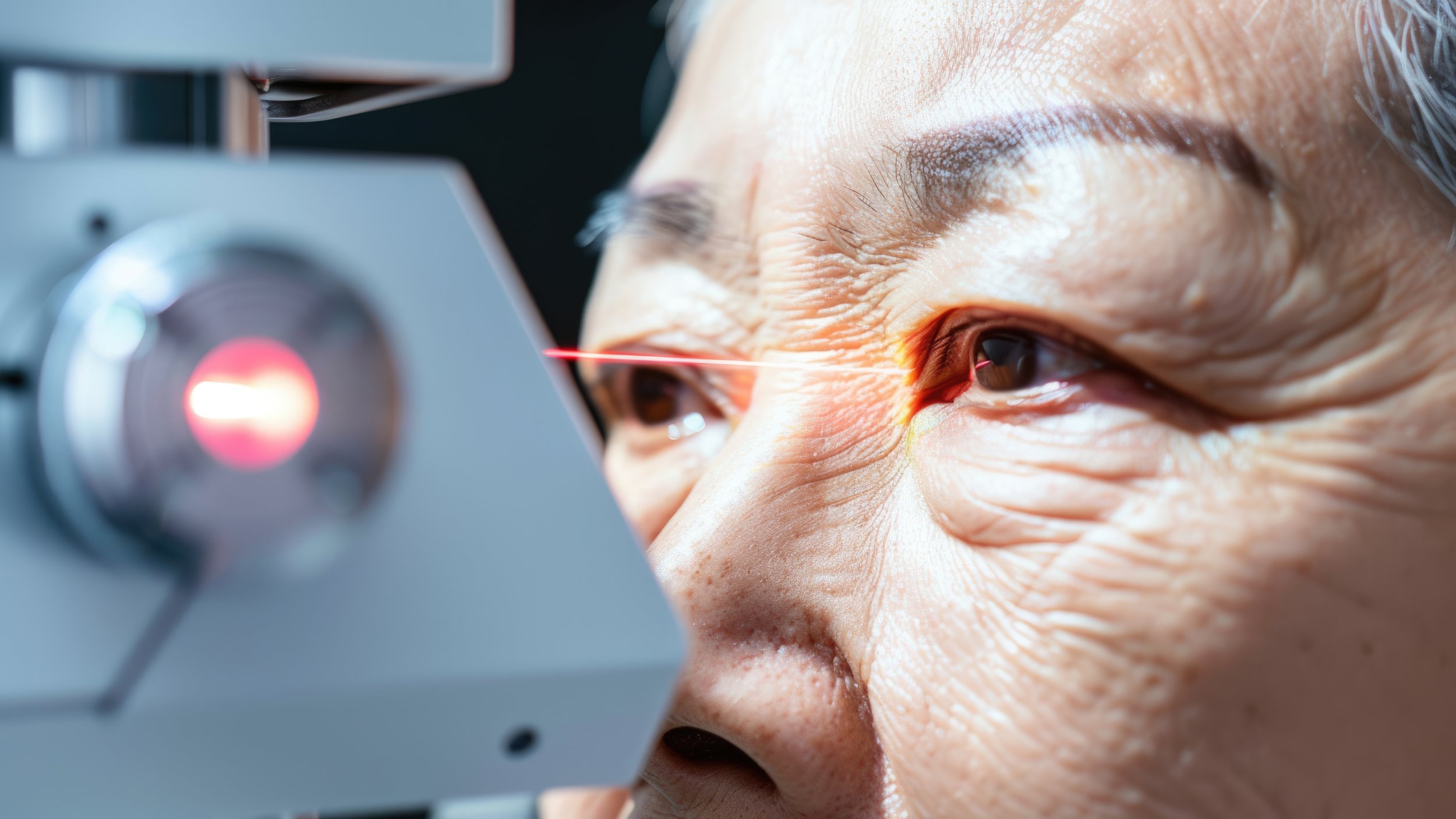
Photobiomodulation
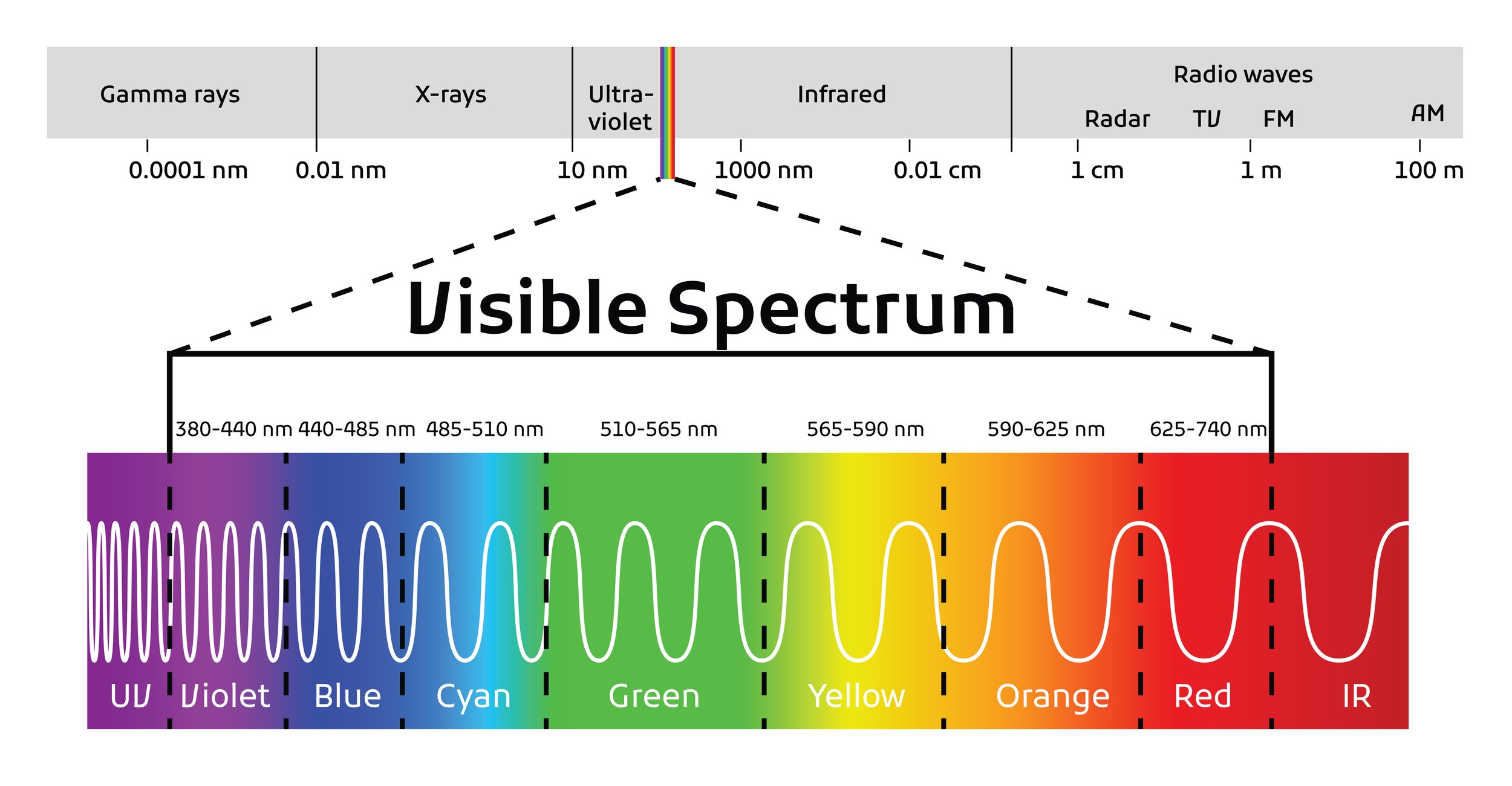
Current research on light therapies and photobiomodulation for treating dry macular degeneration shows promise but remains contentious. Early-phase studies—such as those using the Valeda Light Delivery System in trials like LightSite III—have reported improvements in visual acuity and stabilisation of retinal features (e.g., limited drusen progression) in patients with early and intermediate dry AMD . Researchers propose that specific wavelengths in the far red to near infrared spectrum can stimulate mitochondrial function and modulate inflammatory processes in the retinal pigment epithelium, potentially delaying degeneration.
However, up to early 2025, significant concerns about the validity of the trial results persist. A systematic review and meta-analysis of randomised controlled trials found that while some improvements in best-corrected visual acuity and drusen volume were statistically significant, these changes did not reach thresholds considered clinically meaningful. Moreover, the existing studies are limited by small sample sizes, heterogeneity in treatment protocols, and a high risk of bias that undermines the reliability of the conclusions .
The LightSite III trial, which evaluated photobiomodulation (PBM) for non-exudative age-related macular degeneration (AMD), faced several methodological concerns that raised scepticism about its findings.
One key issue was the small sample size—only 100 subjects (148 eyes) were included, which limited the statistical power of the study. A larger cohort would have been preferable to ensure more robust conclusions. Additionally, baseline differences between the PBM and sham groups created an imbalance, making it difficult to compare outcomes fairly. For example, variations in age distribution and disease severity between groups may have influenced results.
Another concern was the lack of long-term follow-up data. While the 13-month analysis showed some visual acuity improvements, the full 24-month results had not yet been reported, leaving uncertainty about the durability of the treatment effect. Moreover, the higher rate of conversion to wet AMD in the PBM group compared to the sham group (5.4% vs. 1.8%) raised questions about unintended consequences of the therapy.
Ongoing trials, like the larger-scale EUROLIGHT study, aim to address these concerns by providing more robust data across patient populations and treatment regimens .
It may well be that future studies provide evidence for efficacy but, at the time of writing, this we do not believe there is sufficient evidence to provide paying treatment outside clinical trials.
Subthreshold Diode Laser
Subthreshold diode laser treatment is an older experimental intervention to reduce drusen in patients with dry macular degeneration while preserving retinal structure. It is no longer utilised .
Unlike traditional thermal laser photocoagulation, this technique delivers low-energy pulses that avoid creating visible retinal burns, thereby minimizing damage to the retinal pigment epithelium and photoreceptors. The treatment is believed to stimulate RPE repair and enhance the phagocytosis of drusen deposits, potentially slowing disease progression. Early clinical studies demonstrated drusen regression using multimodal imaging techniques such as fundus autofluorescence and OCT, although improvements in visual function remain ambiguous. Safety profiles are generally favorable compared to conventional lasers, yet optimal treatment protocols and long-term outcomes required further validation.